Medical cannabis use and identity: The role of state laws
New state markets could inject an additional $18 billion annually into U.S. legal cannabis market by 2030
February 21, 2023
More Americans Are Seeing Green
March 21, 2023By Dr. Amanda Reiman (Ph.D., MSW), Chief Knowledge Officer, New Frontier Data
One of the defining characteristics of state medical cannabis programs is the list of qualifying conditions. Some states like Ohio, Pennsylvania and Michigan have finite lists of qualifying conditions with additions allowed by the state medical board. Others, such as California, Maine and New York, allow doctors to decide whether cannabis is appropriate for treatment without a finite list of conditions. This patchwork of medical access means that someone with a certain condition would be eligible for medical cannabis access in one state, but not in another, blurring the line between medical and recreational identity among consumers. Indeed, according to New Frontier Data’s consumer survey, over half of consumers consider their use BOTH medical and recreational. But does self-identity as a medical consumer differ from state-sanctioned identity (the ability to obtain a medical card) when it comes to the how much people identify with the label as “cannabis consumer”? And what are the social and environmental pathways for the formation of cannabis identity?
The authors also interviewed several consumers who claim that their use is only recreational in nature to dive deeper into how cannabis identity is formed. Results showed that identity formation is connected to the context of use (initiation, geography and prior knowledge); medical and wellness-based motivations including harm reduction and substitution for other substances; and the adoption of medical or recreational language to describe their experiences. In nearly all cases, those claiming exclusive recreational use described the underpinnings of wellness and medical motivations and outcomes.
While there are many reasons why a state may limit the number of qualifying conditions for medical cannabis access, the result is the blurring of the line between medical and recreational use that varies depending on what state a person lives in and how they experience cannabis as they develop their identity around it. This patchwork of access not only impacts how policies are created and how the industry is implemented. It extends to how consumers view their own use and identities related to cannabis.
This was the topic of a recently published paper in the journal, Public Health in Practice, led by New Frontier Data’s Chief Knowledge Officer Dr. Amanda Reiman, along with co-authors Dr. Josh Meisel, Dr. Rielle Capler and Darcey Paulding McCready. The paper is titled: Medical Cannabis Identity and Public Health Paternalism and is available for free download here.
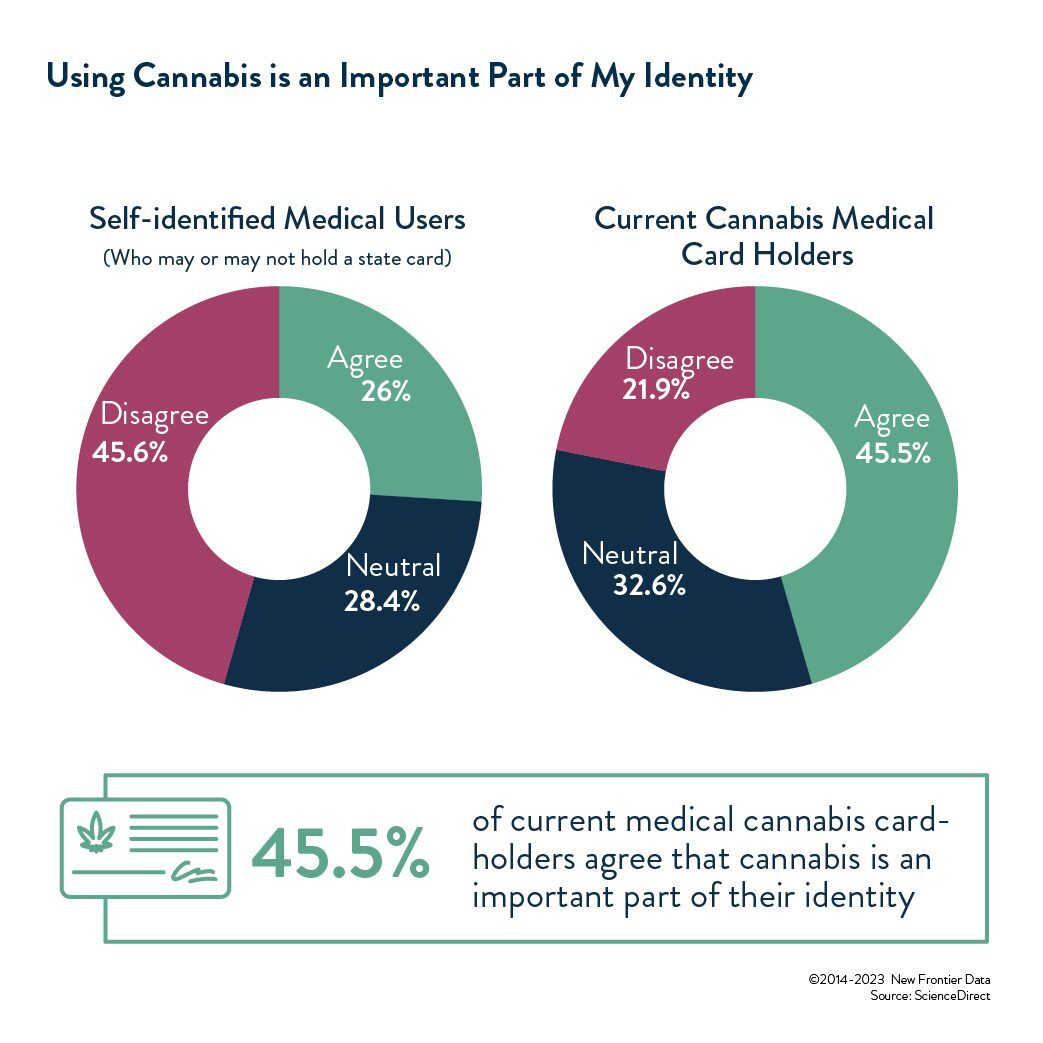
The authors found that self-identity was correlated with state-sanctioned identity, meaning that those who self-identified as only or mostly medical consumers were more likely to have gotten a state-sanctioned medical cannabis card. It was also discovered that those who consider themselves only or primarily medical consumers were over-represented in states that only allow medical use, reinforcing that the state definition of who is a “medical” consumer is correlated with how people identify their own consumption. Furthermore, those with state medical cannabis cards were significantly more likely to say that being a cannabis consumer was an important part of their identity compared to consumers without a medical card, but this was not the case when considering self-identity, where those who self-identify as medical consumers were more likely to reject a cannabis identity compared to those who consider their use both medical and recreational. Finally, those who live in states with finite lists of qualifying conditions were significantly less likely to report having a state medical card than those who live in states with open-ended or doctor-determined lists of conditions.