Popularity of U.S. Medical-Use Markets Far Outpaces Federal Policies
Pain Patients Dominate Medical Cannabis Programs
July 21, 2019
Decline in Medical Cannabis Patient Participation
July 28, 2019By J.J. McCoy, New Frontier Data Senior Managing Editor
As the number of Americans suffering from chronic pain reaches 50 million, an increasing percentage of patients are turning to medical cannabis and reporting extremely strong results, suggesting high growth potential as medical markets expand globally.
In May, the Department of Health and Human Services issued a report by its Pain Management Best Practices Inter-Agency Task Force with recommendations for pain sufferers to function and improve their quality of life. The Centers for Disease Control and Prevention (CDC) plans to update and expand its 2016 chronic pain guidelines with new research, and this fall the Food and Drug Administration (FDA) aims to add warning labels to opioid medications detailing the risks of abruptly stopping the drugs.
Due to federal prohibition, what those agencies have yet failed to do is seriously consider the wisdom of the crowd among 3.7 million Americans currently using medical cannabis.
Having last week reviewed the market saturation rates among states with legalized medical cannabis, recent news of unexpected success for Oklahoma’s medical-use program led New Frontier Data to revisit patients’ reported motives and experiences with it.
According to the National Institutes of Health, among all U.S. adults, nearly 40 million (17.6%) report suffering from severe pain, while about 25.3 million (11.2%) complained of experiencing daily pain throughout the previous three months. Chronic pain is more than an uncomfortable nuisance: People coping with severe pain had worse health, used more health care resources, and experienced more disability than other adults.
As discussed in New Frontier Data’s 2018-2019 Cannabis Consumer Report: Archetypes, Preferences & Trends, the five most common conditions reported among self-identified, medical-use consumers are anxiety (46%), pain (39%), insomnia (27%), arthritis (25%), and migraine headaches (25%), respectively.
Such afflictions have led people to seek the benefits of cannabis, with some finding themselves surprised by the breadth of its impact on their lives. According to the American Legion, 22% of U.S. military veterans use cannabis to treat a mental or physical condition. The group has been lobbying for the federal government to conduct research and consider offering treatment options for its members.
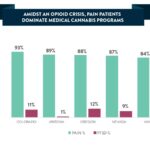
Regarding efficacy, 94% of medical-use consumers say that their condition is improved because of cannabis. Nearly 2/3 (66%) of consumers found that their use of medical cannabis improved their symptoms “significantly”, versus less than 1% finding that their conditions worsened “slightly.” No patients reported that their condition “worsened significantly”.
Furthermore, 70% of medical-use patients chose to substitute cannabis for prescribed medicines, while 73% of all medical-use consumers have chosen to use cannabis in place of some or all other medicine (whether prescription or over-the-counter products). Among all patients, reported improvements from cannabis use were highest for chronic pain (at 97%), and migraines (96%).
A 2017 National Academies of Sciences, Engineering, and Medicine report found consensus among more than 10,000 scientific abstracts suggesting substantial evidence that cannabis is effective in treating chronic pain, in addition to reducing spasticity for multiple sclerosis patients, and mitigating symptoms of chemotherapy-induced nausea: “The committee found evidence to support that patients who were treated with cannabis or cannabinoids were more likely to experience a significant reduction in pain symptoms.”
While motives for people’s medical use of cannabis vary widely across consumer demographics, its application in managing pain is a unifying characteristic. Furthermore, where medical cannabis is legal, and pain an accepted condition for the patient registry (some states do not recognize it as a qualifying condition), pain patients can comprise more than 90% of a given program’s participants.
The large number of consumers already using cannabis to manage pain, and claiming significant benefit from it, is indicative of how national lawmakers have lagged behind public acceptance of the therapeutic value of cannabis. The disparity, coupled with the extraordinary toll that opioid misuse has been taking across the country (despite good news of a recent downturn in opioid-related deaths, it only comes a year after a record number of nearly 17,000 fatal overdoses) serves to heighten the urgency for a comprehensive and pragmatic assessment of the role which cannabis might play in helping mitigate the national public health crisis.